DENTIST'S GUIDE to INFECTION FREE CLINICS
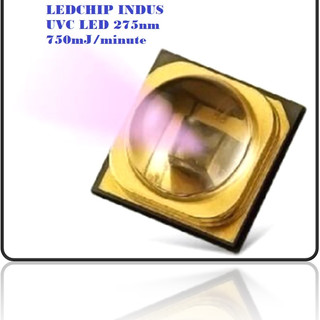
- UVC LED LEDchipIndus K
- Dec 19, 2022
- 18 min read
The ‘new normal’ in post–COVID-19 pediatric dental practiceby Viral Maru First published: 19 June 2021 https://doi.org/10.1111/ipd.12764
Abstract The COVID-19 pandemic has posed an extraordinary challenge to the world. Dental healthcare personnel are considered to be at high risk as they work in close proximity to the oral cavity of patients. New procedures of approach and management should be incorporated in different aspects of routine dental practice. In addition, pediatric dentists are posed with unique and extraordinary challenges of parental anxiety and behavioral guidance of pediatric patients and parents/guardians. The aim of this study was to highlight the changing perceptions of pediatric dental practice as the ‘new normal’ in the post-COVID era. 1 INTRODUCTION Coronavirus disease 19 (COVID-19) marks a significant era from several perspectives. First, it has profoundly affected health globally. Second, there have been numerous socioeconomic consequences. For pediatric dentists, there is a need for revising operating protocols since personnel are in close proximity to patients and are prone to COVID-19 exposure through saliva and aerosols. Such revisions are expected to increase the safety of the patients and the dentists. It is estimated that the COVID-19 pandemic is not expected to end in the short term. The recovery time is expected to be extended. Until the pandemic threat settles down, it is expected that many famlies will defer dental treatment except for emergency treatment or problems that cause significant pain. Individuals may be prone to infections originating from dental practice.1 Among the primary concerns concerning COVID-19, the high potential for viral spread through liquid or aerosol contact during dental procedures is worrying.2 Aerosols are considered as the primary mechanism for COVID-19 spread. Hence, there is a risk of first-line COVID-19 exposure to dentists and other medical personnel.3 Another issue concerning COVID-19 is viral persistence in operating rooms (Figure 1). High-speed rotary instruments could lead to the virus remaining airborne or adhering to surfaces.4 Radiology operators may be at less risk if they remain well protected; nevertheless, the air remains contaminated and therapeutic procedures could potentially expose the operators to COVID-19 when personal protective equipment (PPE) is removed or while healthcare personnel prepare for successive procedures.

FIGURE 1Open in figure viewerPowerPoint Various routes for the spread of infectious agents in pediatric dental clinic setupOn June 3, 2020, the U.S. Centers for Disease Control and Prevention (CDC) provided revised guidelines titled ‘Interim Reopening Guidance for Dental Settings’ for continuing non-emergency dental procedures during the COVID-19 pandemic.5 Specialty bodies and authorities have provided guidance for continuing non-emergency dental practice at the regional and country levels. In India, the Dental Council of India in association with the Ministry of Health and Family Welfare (Government of India) has set forth guidelines for dental practitioners to resume practice during the pandemic.6, 7 The COVID-19 pandemic has led to the modification ofdental practice protocols so that infections may be prevented or controlled. In the context of pediatric dentistry, checklists and guidelines have been approved and set forth by the American Academy of Pediatric Dentistry (AAPD) along with the Royal College of Surgeons of England.8, 9 In addition to an overall set of guidelines to reduce COVID-19 transmission arising from dental practice, pediatric dentistry faces unique challenges in the wake of this pandemic, where a significant challenge is the guidance and behavior management of pediatric patients. In the context of dental clinics for pediatric dentistry, non-pharmacological behavioral guidance methods remain primary. There is a requirement to promote and teach children to develop a positive mindset for maintaining oral health, where there is a need for regular interaction between pediatric dentists, patients, and parents/guardians. The modified practices concerning dental practice for pediatric patients during COVID-19 affect the behavioral guidance issued for routine dentistry. These challenges could lead to deterioration in rapport development, thereby affecting the quality of dental care provided to children. Therefore, the objective of this review was to help establish a ‘new normal’ based on changing perceptions within pediatric dental practice, which will continue to influence practice long after the COVID-19 pandemic subsides.2 GENERAL PRECAUTIONS AND DISINFECTION COVID-19 infection manifests less severely in children compared to adults. However, infected children could remain asymptomatic or have nonspecific and mild symptoms. All individuals who have visited a dental clinic may be potential viral carriers. Therefore, all protocols for preventing virus spread should be followed strictly during routine dental practice concerning pediatric patients. Risk assessment should be performed to determine the level of protection required during a procedure, and appropriate personal protective equipment (PPE) must be used. Typical precautions suggested to prevent virus spread are the use of gloves, wearing aprons, and protecting the mouth and eyes (using masks, goggles, or a filtering facepiece [FFP]). These precautions are followed when there is a chance that the healthcare personnel could be exposed to body fluids from the patient. It is recommended to use ‘disposable’ or ‘single-use-only’ equipments (Tables 1 and 2).10, 11 TABLE 1. Most commonly used various types of PPE10, 11Type of PPEAdvantagesDisadvantagesMedical maskEasy to wear, disposable, and comfortable compared with N95, N99 respirator, or PAPR.Unreliable efficacy against novel influenza or highly virulent droplet pathogens, not indicated when operator is in contact with highly virulent pathogens during the aerosol-generating procedure.Particulate respirators (FFP2, FFP3, N95, etc)Indicated for airborne pathogens, able to protect from virulent pathogens during the aerosol-generating procedure, disposable.Less comfortable, facial hair and facial deformity prevent sealing mask to face.Powered air-purifying respirator (PAPR)Desired for high-risk aerosol-generating procedures, half or full facepiece provides facial protection.Unwieldy, battery-operated, not disposable.GownEasy to put on and take off, not causing heat, disposable, more available.Have more openings than coveralls.CoverallCovers large part of surface area.Causes heat stress unwieldy.ApronAdditional protection when using gowns or coveralls.Disinfection is needed with apron not disposable.GogglesEasy to wear, protection to eyes.Affect visibility with fogging, Some parts of face may not be protected.Face shieldLess fogging, Easy to wear, covers larger part of face.Gloves (double gloving)Reduction in the risk of transmission for high virulent pathogens through glove holes, reduction in contamination risk for hands when removing gloves.Reduction in tactile sensation, unwieldy removal process.Head and neck coverProtects head, neck skin, and hair.No evidence about protection in high-risk.BootsEasy to disinfect, considered a standard equipment in high-risk procedures.Lack of information in comparison between boots vs shoes with cover.Shoes with coversEasy to wear.Not optimal when floors are wet. TABLE 2. Proposed differences in PPE, depending upon the level of risks in various dental proceduresPre-COVID eraPost-COVID eraNon–aerosol-generating dental procedures.
Sterilized headgear.
Protective goggles.
Surgical mask.
Disposable latex gloves.
Disposable or sterilized headgear.
Protective goggles.
Surgical mask.
Disposable or sterilized gown.
Disposable latex gloves.
Aerosol-generating dental procedures.
Disposable headgear.
Disposable/sterilized visor to remove immediately.
Surgical mask.
Disposable gown.
Disposable latex gloves.
Disposable headgear.
Disposable/sterilized visor to remove immediately.
FPP3 / powered air-purifying respirator (PAPR).
Disposable protective suit.
Disposable latex gloves.
Cover shoes.
2.1 Personal hygiene
To prevent the spread of infection, pediatric dentists must maintain personal hygiene. Pediatric dentists must present themselves and their practice as safe and trustworthy so that patients and parents/guardians are comfortable being treated by dentists. Moreover, it is crucial to make the patient feel confident and safe about the procedure because, in this information era, patients have a higher awareness of the treatment and associated risks. Noteworthy hygiene aspects include the following:
If there is a chance of the doctor's hair coming in contact with the patient or the equipment, hair could be tied at the back or a surgical cap could be used
Masks or shields should be used to prevent contact with facial hair
The arms, hands, and the face should be made free of jewelry during treatment
The nails should be of appropriate length to prevent tearing the gloves, while cleanliness is crucial to prevent risks related to accumulated debris
Washing the hands and the entirety of the forearms is crucial both before and after treatment.12
It is crucial to ensure a high level of hygiene, especially concerning the hands because several infectious pathogens in hands that cause diseases such as COVID-19 affect all the individuals involved in a dental procedure. ‘Hand hygiene’ refers to processes performed to eliminate pathogens from the hands:
When washing hands, it should be ensured that soap is used until a rich lather is developed and spread across the hand surface before it is rinsed off
Antiseptic agents may be employed to kill microorganisms. Such agents include alcohol-based sanitizers and antimicrobial soaps, among other agents
Surgical hand rubbing process that eliminates transient microorganisms and flora may be employed for the duration of a dental surgery using alcohol-based hand sanitizers or antimicrobial soaps.13
2.2 Disinfection COVID-19 has genetic similarities with SARS-CoV, which indicates that COVID-19 may probably be handled using 0.5% solution of hydrogen peroxide or 0.1% solution of sodium hypochlorite, phenolic acids, ethyl alcohol (62%-71%), and quaternary ammonium compounds. It is crucial to remain vigilant concerning the usage, duration, and dilution of the substances. Due attention must be given to the expiration time, which indicates the duration for which a solution is effective. Recently, a research paper suggested that 0.1% sodium hypochlorite may be used as a surface disinfectant. Alternatively, ethyl alcohol at 62%-71% concentration may be applied for one minute to eliminate COVID-19.14, 15 Following treatment, it is crucial to ensure that the work surfaces undergo appropriate decontamination using 70% ethyl alcohol (Table 3).16
https://onlinelibrary.wiley.com/doi/10.1111/ipd.12764 TABLE 3. Surface disinfection table10, 11, 16ItemRecommended methodAlternative methodAttachments dental unitsClean with 2% glutaraldehyde and then rinse.Clean with 70% alcoholBracket tables
Clean with 70% ethyl alcohol.
If there is blood or pus, clean, disinfect with 0.5% sodium hypochlorite, and rinse.
Dental chairs
Clean with detergent and water.
If there is blood or pus, clean, disinfect with 0.5% sodium hypochlorite or 2% glutaraldehyde, and rinse.
Dental service unit
Wipe with detergent and water.
If there is blood or pus, clean, disinfect with 0.5% sodium hypochlorite or 2% glutaraldehyde, and rinse.
3 TELECONSULTATION AND TRIAGING The ‘Dental HealthCare Personnel’ (DHCP) refers to dentists, dental hygienists, dental assistants, and receptionists. These individuals are required to keep themselves updated about the skills and protocols concerning infection control. Such information is routinely issued by the relevant authorities to facilitate in preventing the spread of infection. It should be a constant endeavor to have telephonic triage for individuals in need of dental care. In the wake of the current pandemic, teledentistry can go a long way in helping patients. Teledentistry is the field that deals with the end-to-end process of creating a dentist-patient network, sharing information, and arranging for digital consultation, workups, and further analysis.17, 18 The symptoms presented by the patient may be used to judge whether an in-person clinical consultation is necessary. Teledentistry could help the dentists prescribe necessary medication and issue the relevant instructions for home-based care in cases where dental treatment is not urgently required. The American Dental Association (ADA) provides guidelines regarding situations that are considered dental emergencies. Despite having access to the guidelines, the dentists should arrive upon a decision using their analysis on whether a patient is in need of emergency dental care (Table 4).19 Once the decision is finalized and communicated, it may be expected of the patient to visit the clinic, where, as the next logical step, the individual should be examined for COVID-19 symptoms to determine the setting where treatment can be provided. https://onlinelibrary.wiley.com/doi/10.1111/ipd.12764
TABLE 4. Definition of urgent and emergency cases as applicable to pediatric dentistry19Emergency careUrgent careOther urgent care
Uncontrolled bleeding.
Cellulitis or a diffuse soft-tissue bacterial infection with intraoral or extraoral swelling that potentially compromises the patient's airway.
Trauma involving facial bones.
Severe dental pain from pulpal inflammation.
Abscess or localized bacterial infection resulting in localized pain and swelling.
Tooth fracture resulting in pain or causing soft-tissue trauma.
Dental trauma with avulsion/luxation.
Dental treatment required prior to critical medical procedures.
Final crown cementation if the temporary restoration is lost, is broken, or causes gingival irritation.
Biopsy of abnormal tissue.
Extensive dental caries or defective restorations causing pain.
Manage with interim restorative techniques when possible (silver diammine fluoride, glass ionomers).
Replacing temporary filling on endo-access openings in patients experiencing pain.
According to Centers for Disease Control and Prevention (CDC) guidance, patients with active COVID-19 infection should not be seen in dental settings and should be referred for emergency care,20; however, most of the dental offices are dealing with emergencies by following the universal precautions. It is recommended that providers obtain a detailed patient history, where the patients should be administered a COVID-19 screening form that includes the questions specified ahead: (a) whether the patient is presently febrile or had a fever in the last fourteen days; (b) whether the patient had respiratory distress symptoms such as breathing difficulties during the last fourteen days; (c) whether the patient had visited a foreign country in the last fourteen days where transmission of COVID-19 was confirmed, and whether the patient was in contact with individuals who have been to such countries; (d) whether the patient had any contact with an individual confirmed to be COVID-19–positive; (e) whether people having documented respiratory distress or fever (in the last fourteen days) have been in contact; and (f) whether the patient had been to meetings, gatherings, or places where there was close contact with several unknown individuals. It is required to screen any individual who accompanies a child for dental treatment. Patients and caretakers should be provided with guidance to visit a dental clinic only in case of emergencies. This information may be disseminated using social media, messages, and other digital portals. Using teleconsultation, the healthcare provider can determine whether the patient requires a visit to the clinic. Moreover, teleconsultation helps to facilitate the establishment of a rapport between the child and the pediatric dentist, which is advantageous if a clinic visit is required.4 PRE-VISIT BEHAVIORAL GUIDANCE Pre-appointment communication sent to the parents helps them understand what may happen during the first clinic visit. Communication can help the parents alleviate anxiety and help the child prepare for the appointment. Age-appropriate leaflets or digital visual communication may be sent to the parents and the patients in addition to the pre-appointment letter. Such communication may set the right expectations by way of illustrations.1 The ‘tell-play-prepare’ concept may be employed before an appointment to guide pediatric behavior. Video consultations can help the pediatric dentist communicate the procedures to the patient and the parents. Pediatric dentists may provide information about the first clinic visit using video modeling on a doll. Parents may provide similar information at home using toys. Dental visits may be stressful, and children have different coping mechanisms. Therefore, it is suggested that children be made aware of the dentists’ appearance when they are using personal protective equipment, which helps remove the element of surprise.5 WAITING AREA After telephone pre-screening and appointment setting, it is suggested that waiting in common areas be avoided and appointments be spaced out. During teleconsultation, the pediatric dental team should inform the parents that a sibling must not accompany the patient; moreover, only one parent should accompany the child. It is advised that the patient and the guardian visit the dental clinic directly after they step out of their homes. Scheduled stops should be avoided, masks should be worn, hands must be sanitized, and any unnecessary contact with surfaces or individuals must be avoided during transit to the clinic. The guardians may wait outside the clinics or stay in their vehicles. When they are due for the appointment, the patient or guardian may be contacted using a mobile phone. After arriving at the dental clinic, both the patient and the guardian must have their faces covered with masks, or with surgical masks, if available. After the individuals enter the dental clinic, the temperature should be determined using a non-contact thermometer, and an assessment should be made concerning the presence of symptoms consistent with COVID-19. If both patient and parent/guardian do not have a fever (ie, temperature < 100.4 °F)* and do not exhibit COVID-19–specific symptoms, they may proceed to dental care using the recommended preventive measures. Several guidelines suggest that patient waiting areas must be well planned to ensure sufficient social distancing along with other preventive measures. Waiting rooms should have child-friendly infographics that indicate the suggested prevention protocol. Books, toys, and other items that may be hard to disinfect must be removed in order to prevent contamination. Additionally, the waiting area should have a child-friendly ambience to alleviate anxiety and fear. Attractive wall, soothing music, and other techniques may be used to provide a soothing atmosphere.6 DENTAL OPERATORY ROOM Pediatric patients may find the PPE attire uncomfortable, and this can affect the consultation and treatment. Children should be made aware of the dentist's appearance when the pre-appointment consultation is provided. It is suggested to have modified PPE kits that use colors, designs, and other appropriate modifications to make them child-friendly. Non-traditional face shields and colored protective suits are already available. While these modifications can help, it must be ensured that infection control is not compromised. Traditional dentistry often requires non-verbal communication such as hand signals, expressions, and body language; however, verbal communication should be preferred for pediatric dental treatment since PPE kits may restrict the visibility of the face. Pediatric patients, especially younger children, may need the guardian to hold them on their lap during the procedure. Moreover, once the guardian enters the operating room, a new set of gloves should be worn since there may be potential contact with several surfaces during the duration of the procedure on the dental chair. For older and cooperative pediatric patients, only the patient should be allowed in the operatory, except in cases where parents are unwilling or unable to extend effective support. Devices and toys that may be used to distract the patient during the procedure may be employed only if they can be disinfected using the recommended protocol. Audio-visual aids may serve as effective distractions; however, screens, televisions, speakers, and other devices must be placed at an appropriate distance so that they may be effectively sanitized, if required. It is not recommended to use video games, handhelds, or virtual-reality headsets during the procedure. In the context of pediatric dentistry, the patients are often given toys or other rewards. In the present pandemic situation, this practice may be continued with care. Only those items should be provided that may be easily sanitized and provided to the children without contact. Alternatives such as digital appreciation certificates may be used (Figure 2). https://onlinelibrary.wiley.com/doi/10.1111/ipd.12764
FIGURE 2Open in figure viewerPowerPoint Pediatric patient care pathway7 POST-TREATMENT The parents must be informed during the pre-appointment consultation about the care protocol that needs to be followed after the procedure. Email or other electronic communication means should be employed to send the instructions specific to the treatment. Digital payment has widespread acceptability and should be incorporated as the default payment method. Using digital prescriptions and payment help reduce physical contact. Because coronaviruses lose their viability significantly after 72 hours, many organizations have promoted a rotation and reuse strategy. It involves acquiring a set number of N95 masks (at least 5 as per the CDC), which should be used in a rotational manner and allowed to dry for long enough that the virus is no longer viable; however, N95 respirators used during the aerosol-generating procedures or those contaminated with blood, respiratory, or nasal secretions, or other bodily fluids from patients should be discarded. Fumigation is inappropriate for a clinical dental setting; nevertheless, floor mopping and waterline sanitization using 0.1% and 0.01% sodium hypochlorite, respectively, may help reduce the probability of cross-infection. Clinics and hospitals produce biomedical waste that must be disposed of regularly and ideally by authorized biodisposal experts. Pediatric dentists may use mobile cameras to monitor the outcomes using images or videos. Mobile phones ensure sufficient provider-patient confidentiality, and the dentists may also send audio-visual material to the patients to guide them toward better maintenance of oral hygiene. The COVID-19 pandemic has caused a widespread change in the way dental care is delivered. Teledentistry holds immense potential since patients may be attended to without face-to-face consultation.8 PROCEDURAL ASPECTS Procedures that have the potential to produce aerosols must be avoided as much as possible. Some recommendations for reducing viral spread include the use of rubber dams, antiretraction hand devices, high-volume saliva ejectors, and the four-hand technique. Preventive care should be emphasized, where the dentists could use teleconsultation and other electronic means to connect with the patients and inform them of best practices. Moreover, preventive care at home or office, avoiding aerosol-producing procedures, and the use of minimally invasive dentistry are recommended. The use of evidence based biological approaches for caries management in both primary and permanent dentition might be more appropriate under the current and near future circumstances of COVID-19. These include the following procedures: 8.1 Pit and fissure sealants For reducing or reversing non-cavitated lesions forming on the occlusal areas of the teeth, the ADA suggests the use of sealants or sealants in combination with 5% NaF varnish every 3-6 months. Additionally, for approximal contact, the ADA recommends the use of 5% NaF varnish or the varnish used in combination with resin infiltration (repeated every 3-6 months) to stop or reverse carious lesions of the teeth.218.2 Atraumatic restorative treatment (ART) The management of caries for pediatric patients may use ART for both permanent and primary teeth. Additionally, glass ionomer–based ART sealing agents may also be employed for treatment. Meta-analyses and a systematic review concerning the retention of ART-based restorations performed in posterior teeth suggest that single-surface restorations performed using ART have higher survival than multiple-surface restorations in the case of both dentitions. Furthermore, ART-based sealing agents possess high caries-preventing characteristics. Hence, during the pandemic, the treatment of posterior teeth affected by carious lesions may be successfully performed using ART, which has a demonstrated history of success over regular treatment.228.3 Interim therapeutic restorations (ITR) The AAPD recommends interim therapeutic restoration as a non-AGP alternative to ART. Although the techniques used for these procedures are similar, the therapeutic objective differs. ITR could be employed for stopping and helping restore decalcified areas and address caries-specific concerns presented by patients, including uncooperative patients and patients having special care needs. This procedure may also be employed when it is inappropriate to use traditional cavity preparation or restoration techniques, thereby leading to treatment getting delayed. One recommended way to handle several open carious lesions is using a modified ITR procedure comprising stepwise excavation prior to permanent teeth restoration. Proximal lesions treated using ITR have higher chances of successful pulp therapy; however, for non-proximal lesions, the ITR had no significant effect on the success rate. There was no significant difference between the outcomes of vital formocresol pulpotomy and indirect capping of the pulp after ITR.238.4 Hall technique (HT) The Hall technique is non-invasive and is employed for restoration of a carious primary molar that is asymptomatic and non-septic using a way that is suitable for children. This technique is based on the use of a preformed metallic crown (PMC) or GIC to help seal non-pulpal cavities in situ. According to the recommendations, the HT method should be considered for crowing those primary molars, which lack indicators of irreversible pulpitis and present radiographic information consistent with normal dentin presence between the cavity and the pulp space. A space facilitated using an orthodontic separator application for 3-5 days may be required for PMC placement. This process does not require anesthesia and does not require any procedure to remove carious tissue. A published case series reported the success of combining the use of GIC ITR as a diagnostic tool for teeth with deep caries that are asymptomatic or exhibiting symptoms of reversible pulpitis with normal radiographic appearance. Subsequently, after some gap, HT and PMC were performed. It has been suggested in the literature that HT is a straightforward process that avoids drilling and the use of local anesthesia, thereby making it suitable for anxious children. Though there are little data to warrant using HT for treating First Permanent Molar (FPM) firmly, we recommend it as an effective treatment protocol after the pandemic subsides. This recommendation is made considering that HT does not require drilling for straightforward restorations, thereby reducing AGP.248.5 Silver diammine fluoride (SDF) Silver diammine fluoride is used to desensitize teeth in cases of molar incisor hypomineralization or non-carious lesions in the FPMs. This odorless and colorless liquid may also be employed to treat children who are at high risk of carious lesions. Moreover, it may be used for handling deteriorating lesions and for children who exhibit restlessness, an inability to tolerate invasive procedures, or those having some form of health impairment or special health care needs. The recommendations issued by the ADA suggest the use of SDF to stop the deterioration of advanced cavitated lesions present on any area of both primary and permanent teeth. The guidelines suggest using a 38% SDF solution in combination with 5% NaF varnish applied biannually. The silver modified atraumatic restorative treatment is also a promising procedure for handing both permanent and primary tooth cavities (involving dentin) after the pandemic subsides.218.6 Chemomechanical caries removal system (CMCR) This technique was formulated to address the challenges of using an air rotor in the context of pediatric dentistry. Carisolv and Papacarie are promising methods for removing carious lesions that have infected the dentin. These methods are recommended in the post-COVID era. Infected carious dentin can be effectively removed using these methods, thereby facilitating the preservation of the tooth structure.9 INHALATION SEDATION Due to the restriction associated with access to general anesthesia, inhalation sedation can be used as an alternative if non-pharmacological behavioral techniques alone are found to be insufficient. The risks of spread of COVID associated with inhalation sedation have been found to be low. Disposable nasal hoods and tubings should be used for all pediatric patients to minimize the risks of spread of infection.10 GENERAL ANESTHESIA (GA) FOR URGENT CARE It is recommended that pediatric dentists drop all elective treatments, including dental procedures performed under general anesthesia (GA). It is critical to keep the risk of cross-infection at a minimum to prevent viral transmission. Guidelines concerning operating room conditions have been issued for appropriately managing suspected or confirmed positive COVID-19 cases. It is suggested that basic emergency dental facilities be maintained at a regional level. Children meeting the specified criteria should be prioritized for the administration of procedures performed under general anesthesia (Table 5).25
https://onlinelibrary.wiley.com/doi/10.1111/ipd.12764 TABLE 5. Procedures prioritized for urgent treatment under GA25
Sustained trauma to the primary dentition where the child is symptomatic (pain not managed with analgesics, infection not managed with antibiotics or interference with eating), and treatment under local anaesthetic is not possible.
Trauma to the permanent dentition, which needs intervention and treatment under local anaesthetic or sedation, is not possible.
Acute dental infection that is not responsive to antibiotics.
Intractable pain or discomfort, which cannot be managed under local anesthetic.
Facial swelling as a result of dental disease and treatment under local anaesthetic is not possible.
Poor dental health is impacting, or is highly likely to impact, their systemic health, and a decision is made that the benefits of surgery outweigh the risks of bringing a child into the hospital during the COVID-19 pandemic.
Additional needs such as those with learning disability or autism, where dental pain is resulting in self-harm or other disruptive or detrimental behaviours.
Compromised swallow and at risk of aspirating a tooth that cannot be removed under local anesthetic.
11 MEDICALLY COMPROMISED AND SPECIAL NEEDS CHILDREN
Young children having preexisting illness are more vulnerable to complications if they develop any infection due to the tooth not being treated; hence, children having such problems should be considered a priority. Some examples of such complications are bleeding caused by health problems or the use of medications, and higher vulnerability to infection (eg, transplant patient, immunocompromised patients, patients with diabetes, and children prescribed steroids or immunosuppressants or undergoing chemotherapy, including children vulnerable to infective endocarditis). Moreover, children suffering from chronic respiratory illnesses are at very high risk of COVID-19. Other risk factors include premature lung issues and oxygen dependency, cystic fibrosis presenting with respiratory issues, interstitial lung disease during childhood, neurodisability, and asthma.25
The AAPD recommends that facilitating medical consultation for immunocompromised children or those having special healthcare needs must adhere to the appropriate protocols. At the same time, referrals should be provided in time so that hospitals are in a high state of preparedness.
Consultations regarding child safety should be made available for the guardians in addition to providing treatment in a hospital-based dental setting, if feasible. Furthermore, the appointment schedule should be carefully planned so that the first or early appointments are given to the appropriate patients. Based on feasibility, constructing rooms following hospital-level guidelines for air turnover and infection prevention is suggested.12 CONCLUSION
COVID-19 has globally affected pediatric dentistry and is expected to have lingering effects even after subsiding. During the pandemic, the recommended standard practice is to clinically treat only medical emergencies or urgent treatment, while keeping triage at a consultation level. Handling medical emergencies should be prioritized, and elective AGPs should be avoided to the best possible extent. After easing of global restrictions concerning COVID-19, there may be changes to the recommended practices in pediatric dentistry, where the emphasis shall be on prevention.
Why this paper is important to pediatric dentists?
The COVID-19 pandemic has led to the modification of the widely used pediatric dental practices so that infections may be prevented or controlled.
This paper provides a patient care pathway that will form the foundation for the ‘new normal’ in post-COVID era.
This paper provides a brief description of the most preferred pediatric dental procedures in post-COVID era.




Comments